Table of Contents
This is the short version of what a CSF Leak is all about:
The classic symptom is that you have no headache when you are laying down, and an excruciating headache when you are not laying down.
Without the proper amount of fluid in your skull to allow the brain to float as it should, things are getting yanked on that were never meant to be yanked on causing the headache.
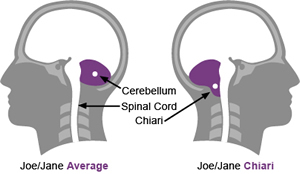
Low CSF fluid levels causes pseudo Chiari, as shown in the drawing.
The detailed explanation of the condition follows:
Cerebrospinal Fluid (CSF) Leaks Explained
By Tracy Moss Stolarski.
 CSF essentially bathes the brain and spinal cord and protects them
from injury and infection. CSF is formed within the inner spaces of
the brain called ventricles. The fluid travels through the ventricles
and exits the brain beneath the cerebellum, which is at the base of
the head. It then travels down the spine, around the spinal cord and
nerves, and back up to the head.
CSF essentially bathes the brain and spinal cord and protects them
from injury and infection. CSF is formed within the inner spaces of
the brain called ventricles. The fluid travels through the ventricles
and exits the brain beneath the cerebellum, which is at the base of
the head. It then travels down the spine, around the spinal cord and
nerves, and back up to the head.
Finally, it passes over the top of the brain where it is absorbed. The fluid is held between the arachnoid and dura membranes. These membranes cover the brain and spinal cord. Leakage occurs when the arachnoid membrane is ruptured.
CSF is a clear, watery liquid that can leak out of the nose, ear, or a head or spinal wound following trauma or surgery. It can occur following a lumbar puncture (spinal tap). Headache is the most common symptom with a CSF leak. Typically, the headache from CSF leak worsens in the upright position {Orthostatic} and is less severe when the individual lies flat {or go away completely}.
A CSF leak is caused by a rupture of the arachnoid membrane. This usually results from trauma, surgery or after a spinal tap. It can also occur spontaneously. Tissue destruction caused by tumors can also lead to a CSF leak.
There is no way to prevent a CSF leak from trauma, lumbar puncture, or surgery. Sports safety guidelines for children, adolescents, and adults can help avoid head injury during sports.
Diagnosis is made by a complete history and physical by a trained health professional. If fluid is actively flowing out of the nose, ears, or a head wound, the fluid can be tested to verify that it is CSF.
Chronic leakage may occur at times following surgery, trauma or spinal tap. Headache and infection are the greatest risks.
Leakage through the nose or ears following trauma usually gets better with rest. Antibiotics are given if an infection is present. If the leakage persists, the health care professional may place catheters in the lumbar spine to reroute the CSF.
Surgical closure of the ruptured membrane is rarely needed. If leakage is caused by erosion due to tumor or infection, the underlying cause must be treated.
CSF leak following a lumbar puncture can be treated with caffeine, and hydration. A blood patch may be placed at the site of the spinal tap. This is a procedure where the individual's own blood is injected at the location of the spinal tap, sealing the hole so as to prevent the leak.
Infection at the site of trauma or surgery may occur. Failure of the rupture to close spontaneously may sometimes occur.
Treatment is usually successful, although complications such as infection can occur.
A person should be monitored for infection and recurrence of CSF leakage. A change of therapy may be needed if infection or recurrence takes place. Any new or worsening symptoms should be reported to the healthcare professional.
INTRACRANIAL HYPOTENSION (IH)
INTRACRANIAL HYPOTENSION (IH) is a condition in which there is negative pressure within the brain cavity. There are several possible causes:
- Cerebrospinal fluid (CSF) leak from the spinal canal
- A leak following a lumbar puncture (spinal tap).
- A defect in the dura (the covering the spinal tube).
- Spontaneous, sometimes following exertion such as swinging a golf club.
- A congenital weakness.
- Following spinal surgery.
- Following spinal trauma.
- Following a shunt procedure for hydrocephalus.
- Lumboperitoneal shunt.
- Ventriculoperitoneal shunt with a low pressure valve.
In some cases, spinal CSF leaks can lead to a descent of the cerebellar tonsils into the spinal canal, similar to a Chiari malformation {Pseudo Chiari}. Large spinal dural defects can lead to herniation of the spinal cord into the defect.
The classic symptom is severe headache when upright, which is relieved when lying flat. Other symptoms can include nausea, vomiting, double vision and difficulty with concentration.
Diagnosis is usually suspected based on the postural dependency of the headache, although in many cases the diagnosis of intracranial hypotension is not considered for some time. A contrast-enhanced brain magnetic response imaging (MRI) scan typically shows thickened and brightly enhancing meninges (pachymeningeal enhancement). Other findings include descent of the thalamus and cerebellar tonsils. Continuous intracranial pressure monitoring is definitive for documenting abnormally negative intracranial pressures. The identification of the site of CSF leak in the spinal canal can be very challenging. In some cases, the site cannot be identified. Methods include:
- Dynamic myelography with fluoroscopy and computed tomography (CT).
- Radioisotope cisternography.
- Spinal MRI.
If the site of the spinal CSF leak can be identified, then options include:
- Epidural blood patch, performed by an anesthesiologist pain management specialist.
- Surgical repair of the defect.
- Over-draining CSF shunts are managed by replacing the valve with one that drains less.
- Lumboperitoneal shunts may have to be removed or ligated.
If the cause of the intracranial hypotension can be identified, the outcome following treatment is good.
SPONTANEOUS INTRACRANIAL HYPOTENSION (SIH)
Spontaneous cerebrospinal fluid leak syndrome (SCSFLS) is a medical condition in which the cerebrospinal fluid (CSF) held in and around a human brain and spinal cord leaks out of the surrounding protective sac, the dura, for no apparent reason. The dura, a tough, inflexible tissue, is the outermost of the three layers of the meninges, the system of meninges surrounding the brain and spinal cord. (The other two meningeal layers are the pia mater and the arachnoid mater).
A spontaneous cerebrospinal fluid leak is one of several types of cerebrospinal fluid leaks and occurs due to the presence of one or more holes in the dura. A spontaneous CSF leak, as opposed to traumatically caused CSF leaks, arises idiopathically. A loss of CSF greater than its rate of production leads to a decreased volume inside the skull known as intracranial hypotension. A CSF leak is most often characterized by a severe and disabling headache and a spectrum of various symptoms which occur as a result of ICH. These symptoms can include: dizziness, nausea, fatigue, a metallic taste in the mouth (indicative of a cranial leak), myoclonus, tinnitus, tingling in the limbs, and facial weakness amongst others. A CT scan can identify the site of a cerebrospinal fluid leakage. Once identified, the leak can often be repaired by an epidural blood patch, an injection of the patient's own blood at the site of the leak, fibrin glue injection or surgery. The clinical syndrome of SIH shares many similarities to the post-lumbar puncture headache. As the name implies, it occurs in the absence of lumbar puncture or central nervous system (CNS) trauma and may be related to the spontaneous dural tears. The International Headache Society recognizes the absence of a definitive pain description for the headache associated with the SIH. In its criteria of 1998, the International Headache Society published the following classification of low CSF pressure , which includes CSF fistula headache: “Posttraumatic, postoperative or idiopathic fluid leak demonstrated by measurement of glucose concentration in leaking fluid, or by leakage of spinally injected dye or radioactive tracer” with characteristics of post-lumbar puncture headache.
According to Khurana, Schaltenbrand first described this syndrome in 1938 using the term “spontaneous or essential aliquorrhea,” emphasizing that it occurs spontaneously, and his terminology implies he attributed the symptoms to the absence of CSF in these patients. Later, the term “hypoliquorrhea” was used. Spontaneous intracranial hypotension is rare, with a prevalence of approximately 1:50,000 persons, and it is more common in women, with female-male ratio of 3:1. Patients with connective tissue diseases {Such as EDS} or Chiari malformation may be more susceptible to SIH syndrome. Postural headache {Orthostatic Headache} is the cardinal feature of the syndrome and should alert the treating physician to the diagnosis. Typically, patients have a sudden onset of headache that is characteristically relieved by lying flat for a few minutes and recurs with resuming an upright position. Other conditions that may cause positional headaches (eg, colloid cyst of the third ventricle, rare cases of migraine headaches) are readily ruled out by MRI findings. The headache in patients with SIH is usually holocranial, though it might be localized to the frontal or occipital head regions. Patients may have additional symptoms, including double vision due to sixth cranial nerve palsy, photophobia, nausea, vomiting, hearing changes, taste changes, malaise, and mental confusion. The mechanism of headache is unclear, but pain could be related to stretching pain-sensitive structures in the cranial vault when the patient is upright because of decreased support by the CSF, which normally keeps the brain floating.
Confirming the diagnosis of low intracranial hypotension syndrome requires imaging studies and CSF pressure measurements, in addition to clinical history. Magnetic resonance imaging {MRI} with gadolinium is critical in diagnosing this syndrome and to rule out any other underlying conditions and should be obtained as soon as the syndrome is suspected and before measuring CSF pressure.
Gadolinium MRI typically shows diffuse nonnodular pachymeningeal enhancement. The mechanism behind pachymeningeal enhancement is related to volume depletion. Decreased CSF volume causes a compensatory increase in blood volume. This is reflected mainly in the venous system and the meningeal veins. There is enhancement of the pachymeninges because they have no blood-brain barrier, contrary to the leptomeninges, which have an intact blood-brain barrier and no enhancement. Diffuse MRI meningeal enhancement can be seen in other conditions, including meningitis, encephalitis, neurosarcoidosis, and meningeal carcinomatosis. Other findings on MRI include occasionally seen subdural fluid collection and descent of the brain. In some patients with SIH, chronic CSF drainage results in sagging and herniation of the cerebellum and medulla through the foramen magnum simulating Chiari I malformation (similar to our patient's condition). However, other findings on MRI (diffuse meningeal enhancement) readily differentiate patients with SIH and tonsillar descent from patients with idiopathic Chiari I malformation. Abnormalities seen on MRI (meningeal enhancement and tonsillar descent) clear or improve substantially with clinical improvement of the headache. In patients with persistent symptoms, spinal MRI, radioisotope cisternography, and computed tomographic myelography can be used to identify the site(s) of CSF leakage, though as in our patient radioisotope cisternography may not show any abnormalities. Nasal packing should be done when radioisotope cisternography is used to rule out CSF leakage through the cribriform plate.
Carefully performed lumbar puncture is critical in confirming the diagnosis and in ruling out any underlying cause for the meningeal enhancement. If SIH is clinically suspected, MRI should be done before obtaining the lumbar puncture, since lumbar puncture by itself may cause meningeal enhancement. In many cases, there will be no spontaneous CSF drainage if CSF pressure is <60 mm H2O. Results of CSF studies are normal otherwise, with occasional mild lymphocytic pleocytosis and an elevated protein value, a finding that may be related to local disruption of the blood-brain barrier.
Recently, a few cases of intracranial hypotension without headache have been described. These cases were seen in few elderly patients after CSF shunt procedure and were diagnosed by typical MRI findings and CSF opening pressure, without evidence of CNS infection or inflammation.
Failure to recognize SIH may subject patients to unnecessary procedures. In many reports, patients with this syndrome have had unnecessary procedures such as repeated lumbar punctures (to rule out infection), meningeal biopsy, and multiple courses of drug therapy before the correct diagnosis was discovered. Once the diagnosis of SIH is established, measures to increase CSF production and increase intracranial pressure should be used to improve the headache. Similar treatment approaches are used in patients with headache after lumbar puncture. Most patients improve spontaneously or with conservative symptomatic therapy with bed rest and increased fluid intake. Caffeine given orally or intravenously is reported to be effective in 75% to 85% of patients with post-lumbar puncture headache. Caffeine is frequently used as first-line therapy in patients with SIH. The mechanism by which caffeine increases CSF production is unclear. Caffeine is an adenosine receptor antagonist that decreases cerebral blood flow and secondarily increases CSF production.
Theophylline is another adenosine receptor blocker that has been used with some success. Analgesics are usually not effective in treating low-pressure headaches. In one study, sumatriptan was found to be ineffective in patients with low-pressure headaches, after failure of conservative management.
Steroids have been empirically used, with variable results. In a minority of patients, symptoms persist and necessitate more aggressive therapy. Epidural autologous blood patch is effective in relieving low intracranial pressure headaches, though previous estimates of epidural blood patch efficacy were overgenerous. Persistent symptomatic relief can be expected in 61% to 75% of patients. In some cases, treatment has been effective even after many months of the onset of headaches. Radiologic improvement in addition to clinical improvement after epidural blood patch has been reported. Complications due to epidural blood patch include infection, chemical inflammation, paresthesias in the lower limbs, neck stiffness, and radicular pain. Another treatment method is continuous epidural saline infusion. Although initially effective, epidural saline infusion is associated with a high incidence of headache recurrence. The majority of patients with SIH respond to conservative and medical therapy, but a few will require a more aggressive diagnostic and therapeutic approach. Using spinal MRI, computed tomographic myelography, and radioisotope cisternography may help determine the site(s) of CSF leak. Intraoperative intradural exploration with saline or dye injection intradurally has been used to identify accessible CSF leakage sites, which can be at any part of the spinal cord. Surgical repair of the leak is rarely used and only if medical therapy fails and there is a clear and accessible source of the CSF leak.
In summary, SIH is a unique medical syndrome with characteristic clinical history and findings on imaging studies. Failure to recognize this syndrome may subject the patient to unnecessary medical treatments and procedures. When diagnosed, excellent outcome can be achieved by symptomatic therapy in most patients.
See also: http://neuropathology-web.org/chapter14/chapter14CSF.html